Creating a culture of belonging in healthcare: Overcoming common barriers
In the complex, fast-paced world of healthcare, where collaboration, compassion, and precision are crucial, cultivating a sense of belonging among staff is more than a cultural goal—it’s essential to delivering high-quality patient care. When healthcare professionals feel seen, valued, and connected within their teams, they are more engaged, resilient, and committed to their work.
A strong sense of belonging starts early—beginning with the interview process. The first few weeks on the job are especially important, as belonging tends to take root quickly and solidifies within the first 90 days. This makes the selection and onboarding experiences pivotal moments for anchoring a lasting connection between employees and the organization.
Belonging in healthcare means that individuals feel emotionally connected to their leaders and broader team, respected for their unique contributions, and aligned with the organization’s mission. It’s also critical to the employee experience—a key component of engagement—and leads to better teamwork, as well as better patient outcomes.
4 ways ‘belonging’ impacts healthcare
A strong culture of belonging directly supports healthcare delivery in several ways.
1. Improved staff engagement and retention
Clinical professionals who feel they belong are generally more engaged and more inclined to stay with the organization. Conversely, Press Ganey’s national engagement data shows that employees who don't feel like they belong are 7.4x more likely to consider leaving.
2. Enhanced patient care
Teams that trust one another, and collaborate effectively, provide safer, more coordinated care. Belonging fosters psychological safety, which encourages people to speak up about safety concerns and introduce new ideas.
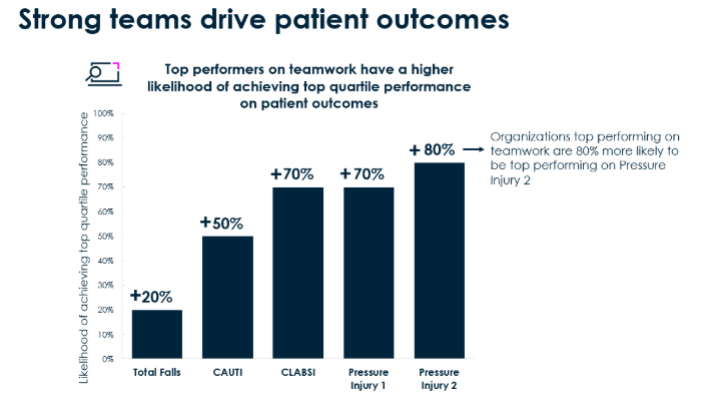
3. Stronger teamwork
Strong interpersonal relationships, mutual respect, and shared values within healthcare organizations foster healthy work environments. When team members feel valued and connected, they’re more likely to support one another and work collaboratively, especially during high-stress situations. In psychologically safe environments, patients rate teamwork higher and experience better outcomes.
Employee experience, patient experience, and clinical outcomes: It’s all connected
Hospitals with staff who rate prevention and reporting high are 3.5x more likely to have patients who say “staff worked together to care for me”—and when patients say “staff worked together,” those hospitals see, on average, 10% fewer falls with injury.
4. Better well-being and resilience
A supportive environment helps reduce anxiety and stress—both of which are common in healthcare roles. Resilient employees are 3x more likely to report acceptable levels of job stress than those with low resilience.
4 barriers to creating belonging in healthcare
Even in a profession rooted in compassion and care, healthcare often struggles to create a true sense of belonging. Leaders must acknowledge and actively address these barriers—not just to improve team morale, but to build a culture where every person feels valued, included, and connected; can be their authentic self; and has the tools to truly thrive.
1. Implicit bias and microaggressions undermine trust
Unconscious bias related to race, gender, age, and/or cultural background, can quietly erode inclusion in the workplace. Team members may find themselves overlooked for opportunities, passed over for promotions, or excluded from key projects. Microaggressions can send powerful messages about who does or doesn’t belong. For leaders, ignoring these issues compromises psychological safety, silences voices, and makes people wonder if they really belong. Ensuring every team member feels seen and respected requires proactive training, behavior modeling, and accountability structures.
2. Workplace silos create division and exclusion
Rigid hierarchies between roles—like physicians, nurses, technicians, and support staff—can quickly become walls. In silos, collaboration flounders, and an “us vs. them" dynamic takes root. When interdisciplinary communication is limited, people may feel sidelined or disconnected from the mission. It’s on leaders to intentionally break down these barriers by fostering cross-functional collaboration, encouraging shared decision-making, and showing, again and again, that great care depends on everyone.
3. Shift work and remote roles can lead to isolation
In healthcare’s around-the-clock environment, rotating shifts, night schedules, and per diem positions can unintentionally isolate team members from the core of the team. They often miss out on team meetings, recognition moments, and casual social interactions that build connection. Leaders must take extra steps to ensure that, across all schedules, the workforce feels included. Strategies like flexible communication, asynchronous recognition, and check-ins that include off-hour staff help ensure no one feels excluded—regardless of their shift or role.
4. Even small exclusions have a lasting impact
Research underscores how deeply exclusion affects team members. A 2019 study found that even one incident of being left out of a conversation, meeting, or decision can significantly erode an employee’s sense of belonging and hurt their performance. For leaders, this underscores the power of everyday inclusion—who's invited to speak, who's kept in the loop, and who’s recognized. Small acts of exclusion can cause lasting harm, while small acts of inclusion can have powerful ripple effects across teams and organizations.
By championing equity, connection, and inclusion at every level, teams become more united, more resilient, and more connected to their shared purpose.
My next article will explore the concrete steps you can take to foster a sense of belonging. For a practical guide on this topic, download our toolkit: “Creating a culture of belonging for your nurses.” If you’d like to discuss how Press Ganey can help bring these strategies to life at your organization, reach out to our consultants.