Using patient experience data to improve age-friendliness
Beginning with CY 2025, CMS introduced an attestation-based measure that signals a deeper commitment to the health and dignity of older adults. The measure— which applies to hospitals, ORs, and emergency rooms— is designed to evaluate how well organizations prioritize improving care for patients 65 years and older. It’s based on the “4 M’s” framework and is structured to address what matters, medication, mentation, and mobility.
What matters, medication, mentation, and mobility
These new measures represent a pay-for-reporting initiative—meaning hospitals receive credit for reporting their measure results regardless of responses to the attestation questions.
Beyond tracking the 4 M’s, the attestation of Age-Friendly Care Leadership requires that hospitals stratify data by demographics and social factors, and use it to drive improvement. Patient experience data is a powerful tool in this effort. It’s a rich source of insight, shining a light on the unique needs of older populations and the extent to which care is currently meeting those needs—or falling short.
In brief
CMS age-friendly hospital measure domains:
- Domain 1: Eliciting patient healthcare goals. This domain focuses on understanding a patient's health-related goals and treatment preferences, which will inform shared decision-making and goal-concordant care.
- Domain 2: Responsible medication management. This domain emphasizes reviewing medication management through monitoring the pharmacological record for drugs that may be considered inappropriate in older adults due to increased risk of harm.
- Domain 3: Frailty screening and intervention. This domain ensures patients are screened for signs related to frailty—including cognitive impairment/delirium, physical function/mobility, and malnutrition—to detect geriatric issues early and intervene where appropriate.
- Domain 4: Social vulnerability. This domain ensures hospitals recognize the importance of social vulnerability screening for older adults and have systems in place to identify and address social issues as part of the care plan.
- Domain 5: Age-friendly care leadership. This domain calls for dedicated leadership—whether an age-friendly champion or an interprofessional committee—to ensure that every aspect of care is consistently high quality.
Overall trust by age and setting
Age-related patterns in patient feedback vary by setting. In the medical practice setting, it’s the younger patients who tend to be the most critical, while overall satisfaction generally increases with age. But there’s an important nuance: Trust—measured by “Likelihood to Recommend” (LTR) the provider or office scores—actually peaks among patients age 65–79, then drops off.
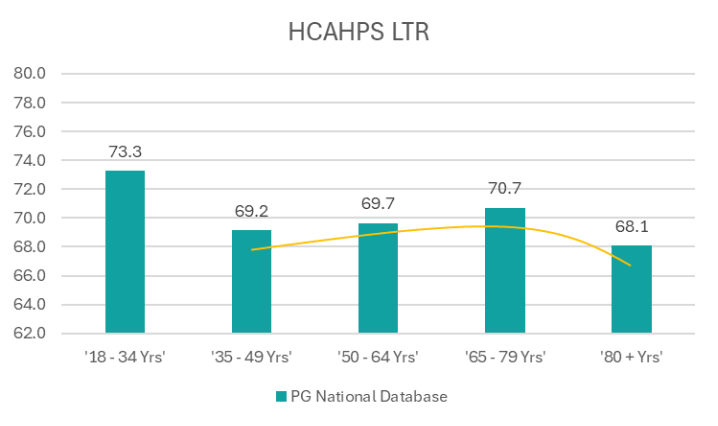
In the inpatient setting, the pattern shifts. Younger patients are, by far, more likely to recommend the hospital. That’s not surprising, as this group often includes maternity patients and individuals in relatively good health (age 18–34), both of which are linked to more positive ratings. But as we move into middle age and beyond, we see the familiar pattern: HCAHPS LTR is lower among patients in the 35–49 range, then evaluations become more positive with age until the early retirement years. Then, they drop off markedly once patients reach their 80s.
Meeting patient needs by age
Looking beyond global measures like LTR helps us pinpoint where care can be more age-friendly.
Younger adults (18–34) evaluate all aspects of care less favorably. Ratings relative to the overall group improve, group after group, up to age 79. Beyond that, average scores are lower across all questions.
Although the differences in experiences for patients in the 80+ cohort may seem small, there is a consistent reversal of the trend toward more favorable assessments with older age. The data, unsurprisingly, demonstrates that everything is more difficult for those 80+. This older age cohort is less likely to feel that things have been explained to them, less likely to feel they’ve been listened to, and less favorable in evaluating process issues, such as ease of contacting the office and wait times at the clinic.
Similar themes emerge in survey data from patients who were hospitalized, but the differences are even more stark. Those in the 80+ range evaluate their inpatient experience less favorably across all measures, often showing sizable negative variation. These patients report particularly low scores in three key areas: feeling ready to be discharged, feeling well informed about their care, and getting timely responses to the call button.
Across care settings, it’s consistently more difficult to meet older patients’ needs in areas like clear communication, education about managing their health at home, and responsiveness. That can make the challenge feel overwhelming—even unsolvable.
But we see meaningful variation in performance across organizations in how well they’re closing these gaps for older patients.
For every measure, some organizations don’t just meet older patients’ needs, but they actually excel. The areas we’ve identified as most challenging for older patients—discharge planning, communication, and responsiveness—have the fewest hospitals showing positive scores. That reinforces just how difficult this work is. But it is possible!
While it’s no surprise that meeting elderly patients’ needs is more challenging, the data demonstrates variation among hospitals, which strongly suggests that improvement is possible.
Benchmarking can uncover where those opportunities are. If, for example, an organization sees lower experience scores among patients over 80, that shouldn’t be dismissed as an inevitable result of demographic trends. Instead, leaders should ask: Is our gap larger than others? Even better: Are there hospitals with no gap at all—and what are they doing differently?
The next step is to dig deeper. We must look at age-friendliness not just at the hospital level, but within individual units and service lines. A “one-size-fits-all” model of care, applied at a hospital level, will most likely result in suboptimal experiences for this demographic. The most impact will likely come from programs designed for the specific needs of very elderly patients—applied on the front lines, where care actually happens.
To learn more about Press Ganey’s solutions that can advance age-friendly care and close experience gaps, reach out to our team.