Transforming healthcare through safety culture
A strong safety culture doesn’t happen by chance. It’s built through trust, consistency, and accountability—nurtured daily through every action and interaction. But new data from Press Ganey’s “Healthcare employee experience 2025” report shows that 2023’s momentum in safety culture stalled in 2024—and organizations will have to recommit to the basics to get back on track.
Safety culture performance is closely tied to workforce engagement—and, in turn, to retention and outcomes. In 2024, engagement fell 0.02 points on a 5-point scale. While 69% of employees remain engaged or highly engaged, the overall decline is cause for concern. Disengaged employees are 1.7x more likely to leave, posing risks to workforce stability, safety, and patient care.
This link between safety and retention is also clear. Employees who don’t perceive a strong safety culture are 1.74x more likely to leave, while those who do report higher engagement—and stay longer. And the benefits extend beyond retention: Strong safety cultures drive better team performance, improved outcomes, and a measurable return on investment that organizations can’t afford to overlook.
Rebuilding safety cultures: From post-pandemic recovery to accelerated results
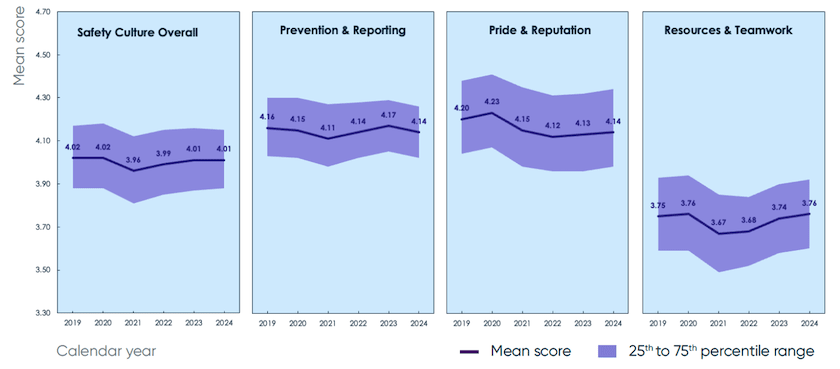
Nearly half (48%) of healthcare workers nationwide have a negative or neutral view of their organization’s commitment to safety culture—a disconnect that directly impacts engagement, retention, and patient outcomes. Safety culture overall did not move. The domain of prevention and reporting declined (-0.03), while pride and reputation (+0.01) and resources and teamwork (+0.02) posted only modest gains. Flat performance at this scale underscores the urgent need for action, as well as the need for leaders to engage their teams and commit to safety.
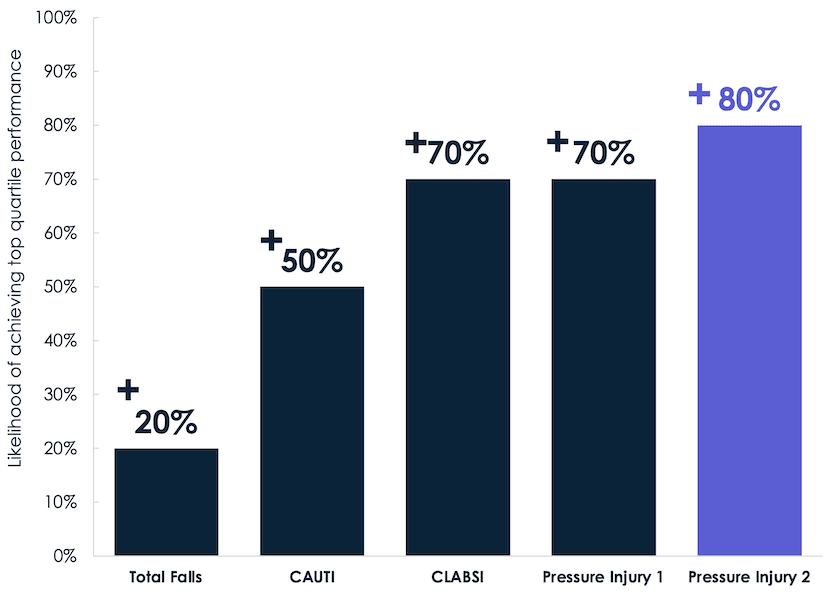
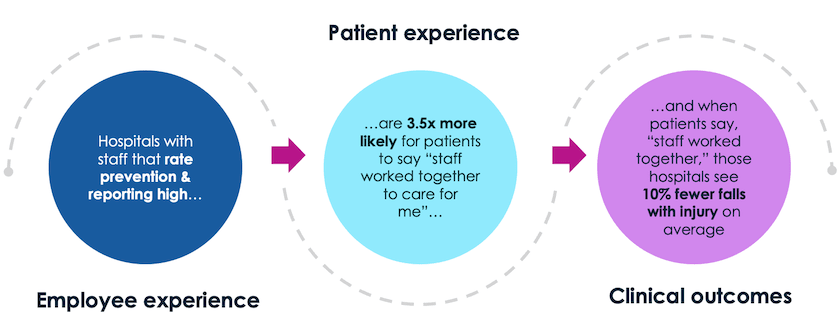
These perceptions reflect deeper cultural and operational challenges. A slowdown is concerning not just for morale, but for outcomes. For example, organizations where employees report strong teamwork on safety culture surveys see significantly fewer adverse quality nursing outcomes, including infections, falls, and pressure injuries.
One of the most powerful levers for improvement in safety culture is building psychological safety—that is, environments where employees feel comfortable speaking up when they see something go wrong, or at risk of going wrong. But a quarter of employees say mistakes are met with blame, instead of treated as learning opportunities. To build a truly safe and highly reliable culture, that response must change.
Leaders must model the right behaviors. They will play a critical role in shifting from a punitive culture to a trust-based one. It starts with responding to safety concerns with curiosity, not judgment. By following up, sharing feedback on changes, and fostering a culture where speaking up is the expectation—not the exception—leaders create the right conditions for psychological safety to flourish.
Social capital as a safety imperative
Strong social capital is one of the clearest indicators of a thriving healthcare environment. Social capital is the value derived from relationships, trust, and collaboration, empowering people to work together effectively and achieve common goals that fuel organizational success. In healthcare, social capital is foundational to building resilient teams and a strong culture of safety. When teams feel safe, supported, and respected, they communicate more effectively and deliver better, safer care.
Without strong social capital, however, teams are more vulnerable to breakdowns in communication, collaboration, and trust. RNs, for example, who report poor teamwork are 1.53x more likely to leave-. When turnover rises, it puts even more strain on already overstretched teams—fueling a vicious cycle where pressure erodes culture, undermines safety, and ultimately harms both experience and outcomes.
The other side of this is a virtuous cycle. Organizations that intentionally build and sustain social capital see stronger retention, a more resilient workforce, and better outcomes. To achieve that, they should prioritize cross-functional collaboration and invest in high reliability organizing. High reliability organizations (HROs) focus on training every employee on universal skills like clear communication protocols, escalation, and cross-checking—practices that strengthen teamwork and build shared situational awareness. When applied consistently, these behaviors not only improve care coordination in the moment, but they also lay the foundation for a more resilient, trusting culture over time.
From good intentions to intentional actions
Healthcare’s challenges are not new. Burnout, inequity, and patient harm have fatigued the system for years. What is new, however, is our ability to listen—as well as the tools we have to understand our workforce and their needs—and operationalize what we hear. When we respond with bold, collective action, we have the power to rebuild trust with our workforce—as well as our patients—and drive real, meaningful change.
This is a call for healthcare leaders to recommit to, and recenter around, safety. By improving psychological safety, building social capital, and ensuring leadership accountability, we can create environments where people want to stay, teams thrive, and we further our mission of zero harm.
Download Press Ganey’s “Healthcare employee experience 2025” to explore the link between safety and the employee experience in greater depth. Or reach out to a Press Ganey expert to discuss your organization’s challenges.